Research > Focus C > Work Packages C01
Summary
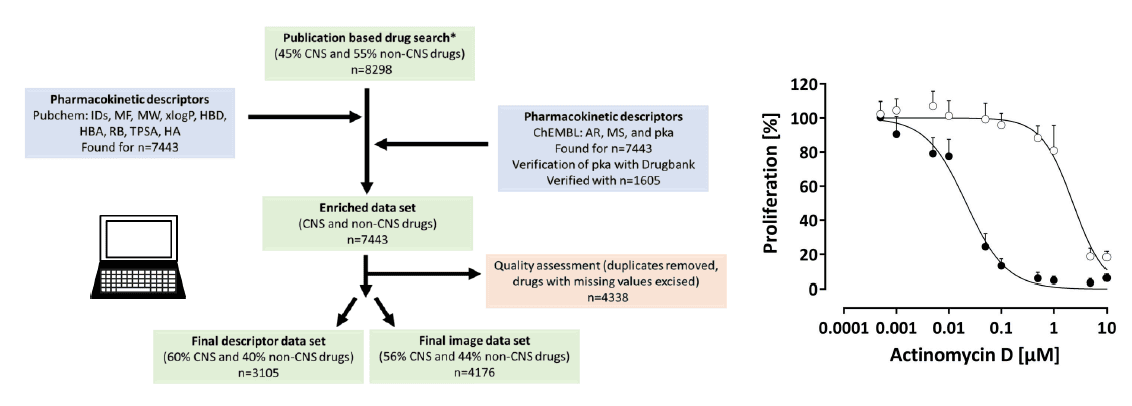
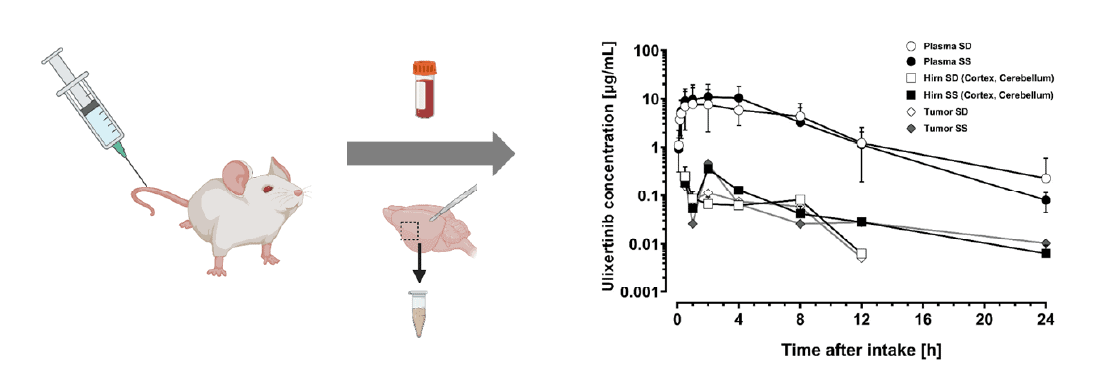
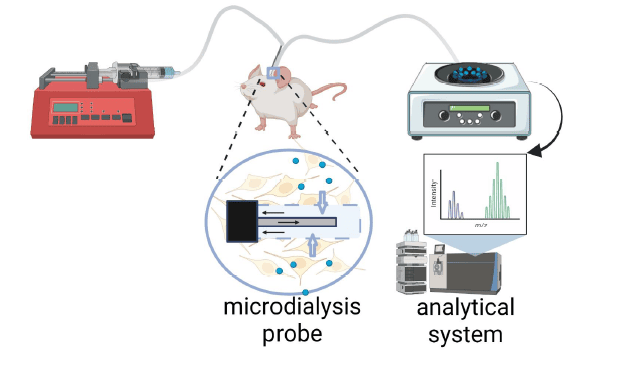
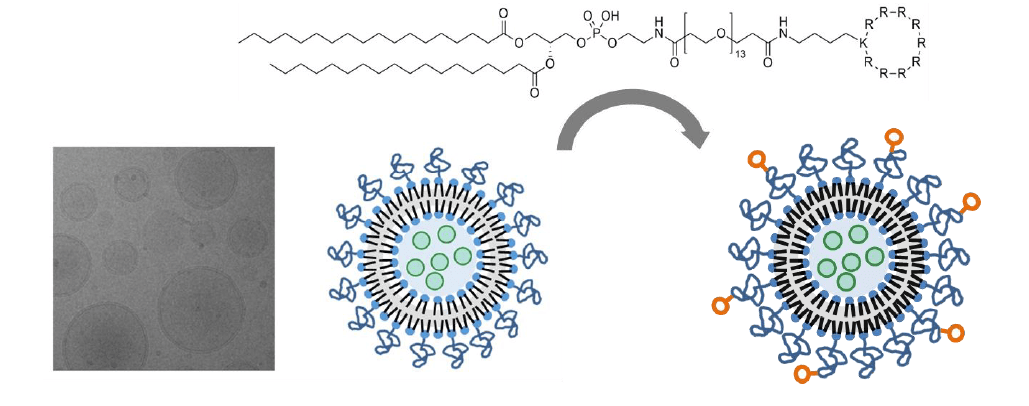
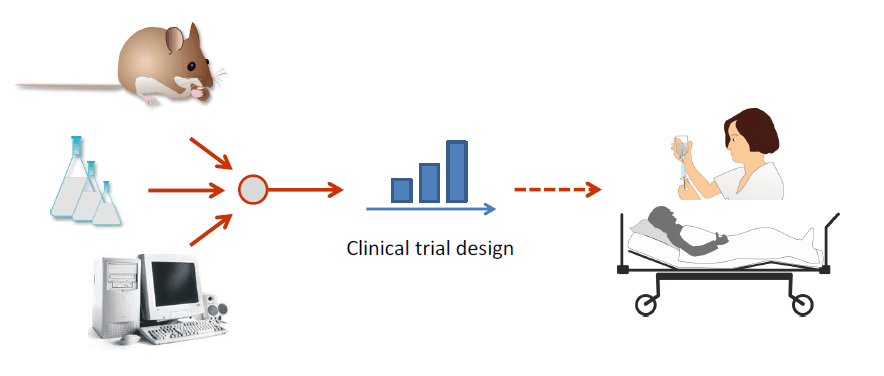
In order to prioritize the preclinical development of drugs & biologicals (and combinations thereof) according to their pharmacological characteristics, we will screen potentially effective drug candidates for their brain accessibility and confirm blood-brain-barrier permeation in vivo and over time using microdialysis. Drug candidates with insufficient brain access will be subject to drug-delivery development using cell-penetrating liposomes for packaging, which will be re-evaluated for their brain accessibility. Final efficacy evaluation of promising drugs and drug delivery candidates will be based on the UNITE Core Collection of orthotopic preclinical models of different molecular subgroups of glioblastoma.