Research findings related to UNITE work package A03
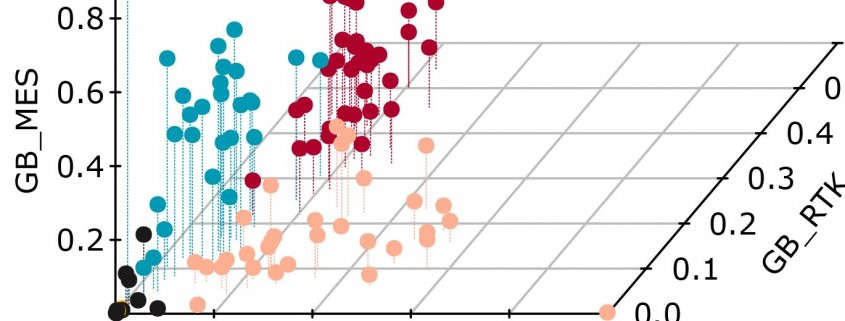
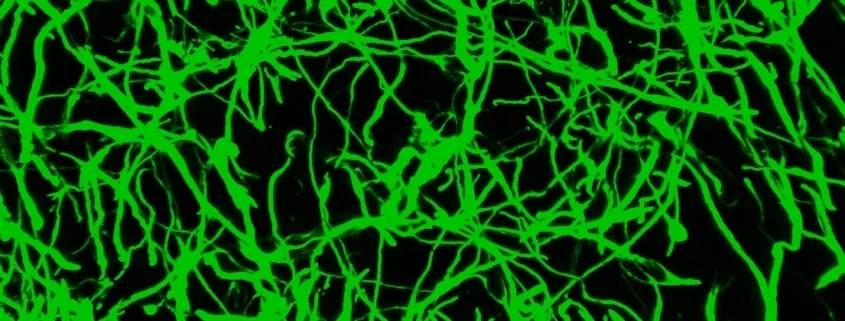
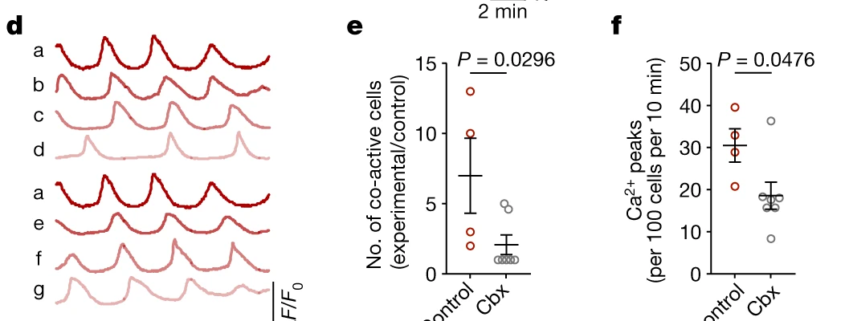
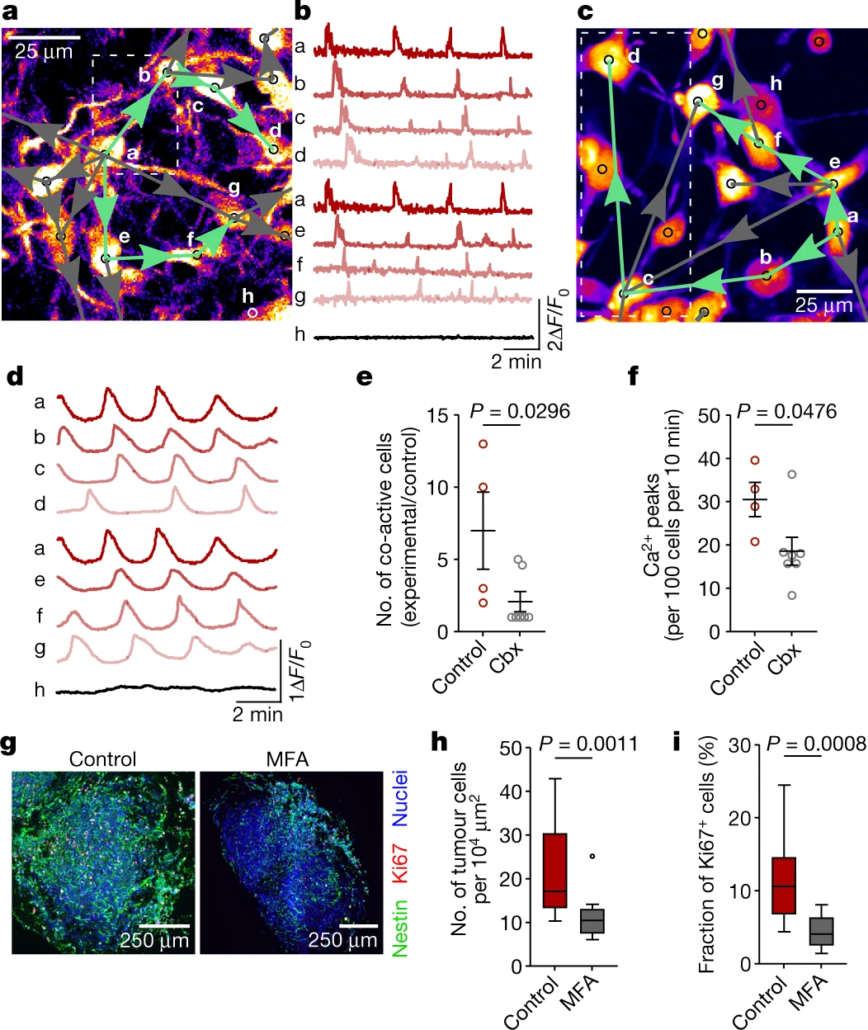
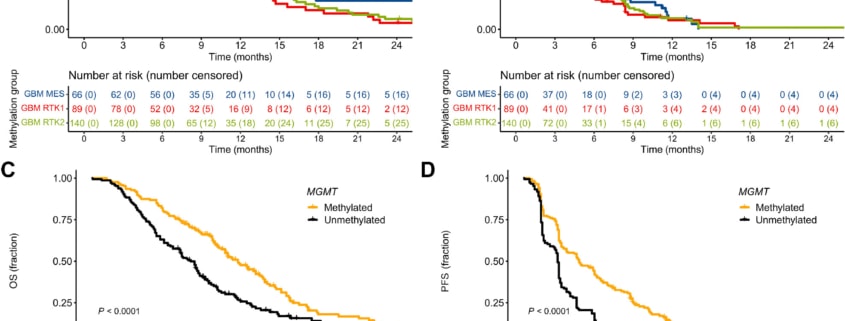
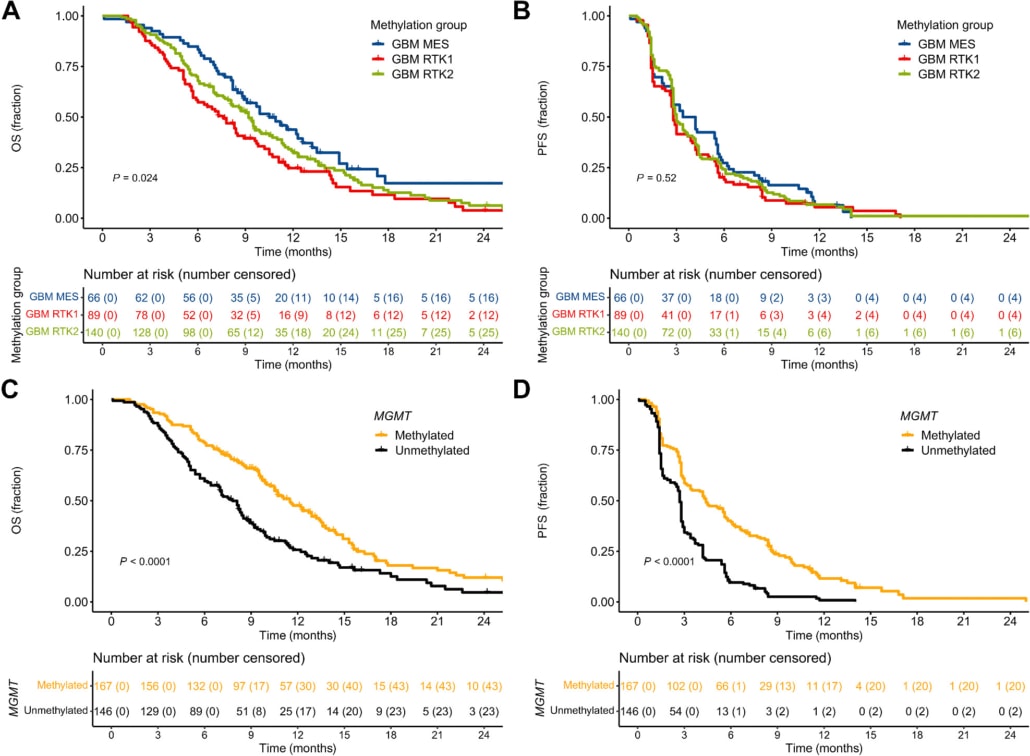
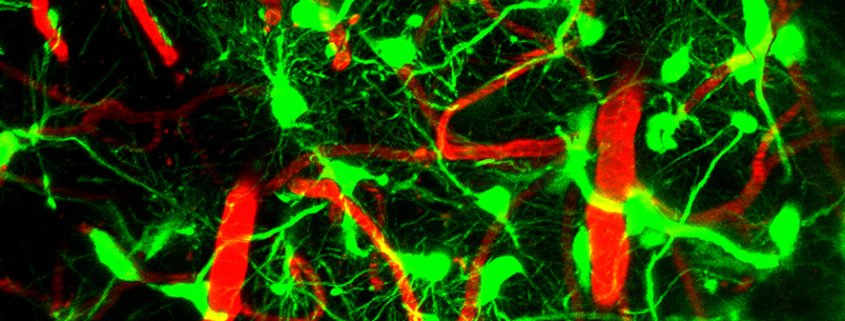
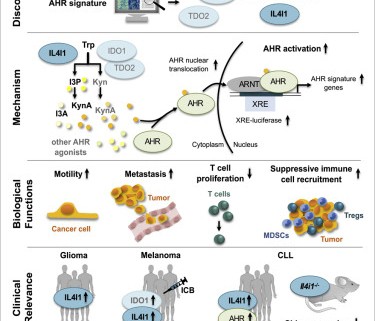
Tumor microtubes (TMs) connect glioma cells to a network with considerable relevance for tumor progression and therapy resistance. However, the determination of TM-interconnectivity in individual tumors is challenging and the impact on patient survival unresolved. Here, we establish a connectivity signature from single-cell RNA-sequenced (scRNA-Seq) xenografted primary glioblastoma (GB) cells using a dye uptake methodology, and validate it with recording of cellular calcium epochs and clinical correlations. Astrocyte-like and mesenchymal-like GB cells have the highest connectivity signature scores in scRNA-sequenced patient-derived xenografts and patient samples. In large GB cohorts, TM-network connectivity correlates with the mesenchymal subtype and dismal patient survival. CHI3L1 gene expression serves as a robust molecular marker of connectivity and functionally influences TM networks. The connectivity signature allows insights into brain tumor biology, provides a proof-of-principle that tumor cell TM-connectivity is relevant for patients’ prognosis, and serves as a robust prognostic biomarker.
Ling Hai, Dirk C. Hoffmann, Robin J. Wagener, Daniel D. Azorin, David Hausmann, Ruifan Xie, Magnus-Carsten Huppertz, Julien Hiblot, Philipp Sievers, Sophie Heuer*, Jakob Ito, Gina Cebulla, Alexandros Kourtesakis, Leon D. Kaulen, Miriam Ratliff*, Henriette Mandelbaum, Erik Jung, Ammar Jabali, Sandra Horschitz, Kati J. Ernst, Denise Reibold, Uwe Warnken, Varun Venkataramani*, Rainer Will, Mario L. Suvà, Christel Herold-Mende*, Felix Sahm*, Frank Winkler*, Matthias Schlesner*, Wolfgang Wick* & Tobias Kessler*. A clinically applicable connectivity signature for glioblastoma includes the tumor network driver CHI3L1. Nat Commun. 2024 15, 968. * UNITE Principal Investigators
 UNITE
UNITE
 UNITE
UNITE